Chapter 2
An Overview
Cytokines secreted by activated immune cells can provoke the moods, behaviors and thoughts characteristic of depression and schizophrenia. Cytokines can also cause the neurotransmitter, hormone and other physiological abnormalities found with depression. Instead of ignoring these landmark discoveries the way establishment psychiatry does, this book incorporates them into psychiatry's current models of depression. This creates a new paradigm of depression we will call The Immune-Cytokine Paradigm of Depression (immune-cytokine POD). The new knowledge on cytokines doesn't replace psychiatry's current insights into depression, but rather it supplements and unifies psychiatry's current view of depression. Figure 1 shows the establishment's Current Paradigm of Depression (Current POD). Figure 2 adds the new information on cytokines for the Immune-Cytokine POD. These two figures will be used to compare and contrast the Current POD with the Immune-Cytokine POD.
Psychiatry's Current Paradigm of Depression (Current POD)
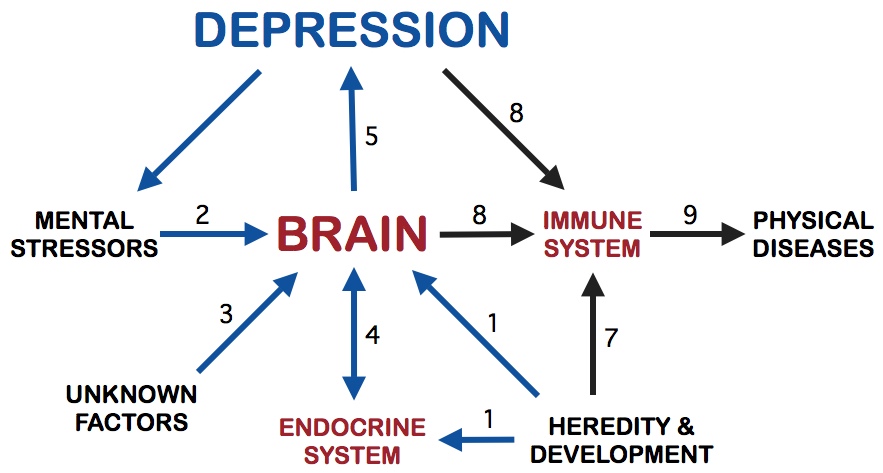
Figure 1. Psychiatry's Current Paradigm of Depression
Let's look at Figure 1 for a moment. It diagrams the basic concepts of depression found in psychiatry's Current POD. The arrows show how the various systems and the brain interact. The numbers on the arrows loosely approximate a possible sequence of events in the development of depression. They are also useful in identifying the arrows for discussion.
Etiology of Depression
The Current POD includes heredity as part of the cause of depression. Depression tends to run in families. The genes from your mother and father determine your innate vulnerability to depression. The exact mechanism by which heredity affects the incidence and severity of depression is not known. But it is known that heredity profoundly influences endocrine and brain function and both of these systems play key roles in depression. It is estimated heredity accounts for about 30 to 50% of the incidence of depression. In Figure 1, the two arrows numbered 1 show the significant influence of heredity, via the brain and endocrine system, on the susceptibility to depression. Notice in the diagram that there is an arrow going from the endocrine system to the brain and from the brain to depression. Thus, anything affecting the brain or the endocrine system will affect the incidence and severity of depression.
Heredity, to a very great extent, also determines immune system function. But, in psychiatry's Current POD, the immune system doesn't communicate with the brain or any structure influencing depression. Hence, in psychiatry's current depression models, heredity's sway over the immune system does not influence depression. In Figure 1, these relations are shown by arrow 7 going from heredity to the immune system and by arrow 8 going from the brain to the immune system. Notice that arrow 8 does not go from the immune system to the brain. In sharp contrast, the Immune-Cytokine POD incorporates the powerful control the immune system has over the brain. This is one of the key ways the Current POD profoundly differs from the Immune-Cytokine POD.
According to psychiatry's Current POD, mental stressors are involved in causing depression. Mental stressors presumably alter some of the brain's neurotransmitters (serotonin and norepinephrine) to produce depression in genetically vulnerable people. Clearly, mental stressors are not the only causes of depression, since vast number of people throughout the world are subjected to severe mental stressors without developing depression. Indeed, mental stressors may only be a minor cause of depression. In Figure 1, the role of mental stressors in altering brain function in persons genetically vulnerable to depression is shown by arrow 2.
Modern psychiatry fully admits that the etiology of depression is, for the most part, unknown. In the Current POD, the forces causing depression are mysterious, unfathomable and continue to be unknown even after a century of biomedical research. Arrow 3, pointing from unknown factors to the brain, acknowledges the Current POD's lack of insight into the etiology of depression.
There may be many reasons why the etiology of depression remains unknown after all these years. As discussed in Chapter One, we suggested that the establishment's classification of depression as a mental disease prevents progress on understanding the etiology of depression. The Current POD doesn't allow a physical stressor to be considered as a cause of depression, because depression is classified as a mental disease. Mental diseases are assumed to have mental causes, physical diseases to have physical causes. There is nothing in the Current POD that can accommodate physical stressors. In the Current POD, except for the endocrine system, the brain is cut off from the rest of the body.
In the Immune-Cytokine POD (Figure 2), a mechanism for physical stressors in the etiology of depression is easily accommodated by the immune system's link with the brain and endocrine system. The connection between the immune system and the brain puts the brain in direct contact with the rest of the body. There is nothing scientifically unusual about this. Physical stressors always activate the immune system and increase cytokine secretion. The immune system and cytokines always inform the brain and endocrine system about serious physical stressors. In the Immune-Cytokine POD, physical stressors take the place of the unknown factors in the Current POD.
Depression can be a cause of depression. It can feed upon itself. The symptoms of depression, such as fatigue, depressed mood, lack of interest and pleasure in things, irritability, social withdrawal and inability to concentrate, tend to make the quality of life worse. With these symptoms, conflicts with family, friends and coworkers will go up, while job performance and satisfaction with family and friends will go down. Some of the sad outcomes of depression are job loss, alienation from family and isolation from friends. Addictive substances become more attractive, because they make the horrible emotions of depression seem a little better for a short period. In this way depression causes psychological, social and economic stressors (i.e. mental stressors) to increase. Misery begets misery. The sixth arrow, going from depression to mental stressors, points out the phenomena of depression helping to induce more depression. A vicious, depressing cycle.
On the other hand, with the modern resources available, depression, instead of making depression worse, can also be self-correcting. If a depressed person recognizes his illness and seeks professional help, then the depression may attenuate. Psychotherapy may help by providing techniques to cope with mental stressors, thereby alleviating some depression. Antidepressants very often improve the symptoms of depression.
Summing up What does the Current POD say about the etiology of depression? Actually very little. Heredity plays a role, but the mechanism is not understood. Mental stressors probably contribute to depression, but there is general agreement that mental stressors are not the main causes of depression. This leaves unknown factors as the mysterious etiologic agents. Unfortunately, the Current POD puts severe restrictions on the unknown factors. Physical stressors are not allowed as causes of depression. The Current POD is not a helpful model. If anything, it profoundly impedes the search for the causes of depression.
Pathophysiology of Depression
The Current POD does have some things to say about the pathophysiology of depression. Most of the insights have been due to pharmacology. The accidental discovery of the antischizophrenic drug chlorpromazine (Thorazine) in 1952 started the triumphant march of psychopharmacology. This event led to the discovery of tricyclic antidepressants a few years later. The search for the mechanism of action of these drugs became intense. It was hoped that the nature of mental illness would be revealed along with clear pathways for the prevention, treatment and cure of these diseases. These hopes have yet to be fulfilled, nevertheless, the search did lead to better drugs for treatment. In addition, neurotransmitter dysfunctions became the prime focus of the search for the pathophysiology of mental illness.
Neurotransmitter dysfunction is biological psychiatry's central concept for the pathophysiology of depression. Serotonin and norepinephrine dysfunctions are the leading candidates, although problems with acetylcholine and dopamine function are thought by a number of researchers to be of critical importance. Almost all the insights have been gained through studying the actions of antidepressant drugs. The actions of the drugs are complex and many, many secrets await discovery.
There is a well documented relationship between the brain and the endocrine system. Neurotransmitters have profound effects on the release of stress hormones and likewise, stress hormones have significant effects on neurotransmitters and mood. This means there is a two way communications pathway between the brain and the endocrine system, as shown by arrow 4. Essentially, the brain can stimulate the production of stress hormones and stress hormones return through the blood to affect the brain. The elevated level of stress hormones usually found in depressed patients is strong support for the importance of the brain-endocrine system relationship in depression. The pathophysiology of the endocrine system during depression is intensively studied by biological psychiatrists.
The brain is at the center of the Current POD diagram. All the arrows pointing to the brain (heredity, endocrine system, unknown factors and mental stressors) are presumably causing neurotransmitter dysfunctions. The neurotransmitter dysfunctions, it is believed, produce the symptoms and signs of depression, as indicated by arrow 5.
Notice that in the Current POD, the immune system does not point to the brain to help cause depression. Establishment psychiatry completely ignores the effects of cytokines on the pathophysiology of the brain. In addition, the powerful effects of the immune system on the endocrine system are disregarded as are the effects of hormones on the immune system. Clearly, the absence of immune system input in the pathophysiology of depression leaves a gaping hole in the Current POD.
Consequences of Depression
Patients with depression have very high rates of physical illnesses. Furthermore, depression appears to increase the severity of physical illnesses. For example, heart attack patients who develop depression have higher death rates and more complications than heart attack patients without depression. The same is true for kidney disease and rheumatoid arthritis. Thus, depression is thought to have very serious consequences.
The Current POD claims depression causes the higher incidence and severity of physical illness by suppressing the immune system. The two arrows numbered 8 illustrate the idea of depression suppressing the immune system. The suppressed immune system then permits more physical diseases to occur (arrow 9).
The notion of depression suppressing the immune system is based on limited and selective immunological reports. The recent extensive publications on immune activation and increased cytokine secretion in depression, make the theory of depression caused immunosuppression very unlikely. This makes the theory of depression caused physical illness very improbable also. We will see in the Immune-Cytokine POD, the reverse is more likely, that is, physical illnesses probably cause depression.
Some Comments The one-way arrow from the brain to the immune system is a very important aspect of the current paradigm of depression. It has fundamental implications for the etiology, pathophysiology and perceived consequences of depression. The concept is based on biological knowledge available before 1979, which said that the communications pathway between the brain and the immune system is a one-way street, going from the brain to the immune system. The biological knowledge available before 1979 also said that there is no communication in the other direction, that is, from the immune system to the brain.
Cytokines were officially recognized and named by immunologists in 1979.1 By 1982 it was established that cytokines could communicate with the brain. Thus, in terms of the immune system-brain relationship, the Current POD is fifteen years out of date.
The Immune-Cytokine Paradigm of Depression
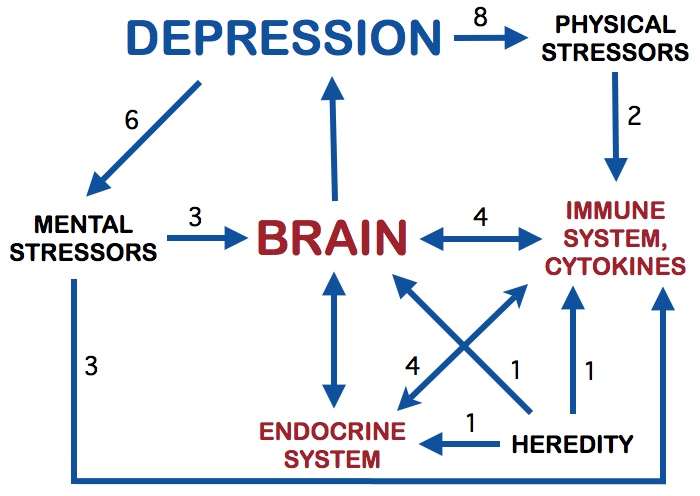
Figure 2. Immune-Cytokine Paradigm of Depression
The Immune-Cytokine POD is diagrammed in Figure 2. It has a number of fundamentally unique features. The first and possibly the most important feature: the communications pathway linking the immune system with the brain is a two-way street. This is not speculation, but rather, since 1982, a well established two-way system. The immune system, via the secretion of cytokines, has a powerful ability to affect brain function. The brain, via the secretion of various chemicals and direct nerve connections with the immune system, has a potent ability to affect immune system function. Therefore, the linkage between the immune system and the brain is a two-way communications link.
The second unique feature: the immune system has a well documented two-way communications link with the endocrine system. This is very important, because endocrine activation is a common finding in depression. Third: physical stressors (infection, trauma, cancer, organ dysfunction, autoimmune disease and physical diseases of any sort) activate the immune system, causing increased cytokine secretion. This, of course, is not new to immunology, but it is a very new addition to psychiatric models of depression. The cytokines are carried to the brain, where they help produce the symptoms and signs of depression. The Immune-Cytokine POD is the only model that explains how physical stressors can cause depression, thereby solving one of the great mysteries of psychiatric disease. Physical stressors replace the unknown factors found in the Current POD.
The fourth unique feature: animal and recent human work has shown that mental stressors activate the immune system and increase cytokine secretion. Therefore both mental and physical stressors activate the immune system and increase cytokine secretion. This makes it possible for the immune system to be the fundamental mediator of stress, whether the stress is physical or mental.
Etiology of Depression
In the Immune-Cytokine POD, heredity profoundly shapes the endocrine system, the brain and the immune system (the three arrows numbered 1), the same as in the Current POD. They do differ in one major aspect: in the Immune-Cytokine POD, the immune system does affect brain and depression. Hence, in the Immune-Cytokine POD, heredity takes part in the etiology of depression through all three systems, that is, via the brain, the endocrine system and the immune system.
Development is also very important in determining how the brain, endocrine and immune system function. From gestation onward, heredity forcefully molds development. In addition, many environmental factors can affect development, such as, mental and physical trauma, infection, medications, addictive substances, toxins and malnutrition. The majority of environmental factors affecting development work through the immune system. Indeed, environmental factors more powerfully shape the development and function of the immune system than any other system in the body. Thus, in terms of heredity, development and the etiology of depression, the addition of the immune system in the Immune-Cytokine POD is extremely important.
Physical stressors, in the Immune-Cytokine POD, are the principal causes of depression (arrow 2). Physical stressors include bacteria, virus, fungus or any other infectious agent. Trauma, organ dysfunction, cancer, foreign antigens, atherosclerosis, autoimmune disease, toxins, dying tissue are additional examples. Physical stressors are the main activators of the immune system An activated immune system, via the release of cytokines, produces most of the symptoms and signs of disease, both physical and mental, especially depression.
Increased cytokine secretion is one of the most important actions taken by an activated immune system. When cytokines are released they act like potent hormones on neighboring cells. If enough cytokine is released, it will migrate through tissue spaces and enter the blood. Once in the blood, cytokine can affect every tissue and organ in the body, including the brain and endocrine system. Arrows numbered 4 show this relationship.
The idea of mental stress impairing the immune system has been a popular one. Nevertheless, recent studies on animals and humans have revealed that mental stressors activate the immune system and increase cytokine secretion. Mental stress also affects various brain centers linked with depression, but this has been known for many years. Arrows numbered 3 indicate the effect of mental stress on brain and immune system.
As mentioned in the previous section on etiology, depression can cause more depression by enhancing mental stressors. In this model, depression could intensify physical stressors. In severely depressed persons, neglect of proper eating, exercise and health care could impair physical heath, thereby increasing the severity of the physical stressors (arrow 8).
Summing up What does the Immune-Cytokine POD say about the etiology of depression? Certainly it doesn't solve the problem of etiology, but it does provide a mechanism to search vast new areas for the causes of depression. First, the effect of genes and development on the immune system is a legitimate place to look for the cause of depression. Second, the vast domain of physical diseases is now open for exploration on the etiology of depression. Of keen interest here are chronic infections, since depression is a chronic rather than an acute disease. Acute infections are easy to identify via sudden onset, fever, overt inflammation and blood work. Once an infection becomes chronic, it is usually very difficult to find. Normally it is hidden someplace in the body and not accompanied by fever and overt inflammation. Unless someone is looking specifically for a chronic infection, blood work will usually pass as normal. In Chapter One, we mentioned the story on peptic ulcer: it took over 50 years to discover it was caused by a bacterial infection rather than mental stress. Think about that.
Pathophysiology of Depression
The Current POD incorporates important discoveries on the pathophysiology of depression, namely, neurotransmitter dysfunction and activation of the endocrine system, especially stress hormone release. The addition of the immune system remarkably compliments these discoveries. Immune system cytokines cause neurotransmitter dysfunction and endocrine system activation, especially stress hormone release (arrows numbered 4). There is also evidence that cytokines can function as neurotransmitters in the brain. Some of this information has been known for over 15 years. Thus, the Immune-Cytokine POD merely replaces an obsolete model of the pathophysiology of depression.
Consequences of Depression
In the Immune-Cytokine POD, we still have to deal with the same facts on physical illness, that is, depressed persons have more physical illnesses and of greater severity than non-depressed persons. The Current POD interprets these facts as evidence that depression causes physical illness and makes them more severe. By comparison, built into the structure of the Immune-Cytokine POD is the notion that physical illnesses are the major cause of depression and more severe physical illnesses should cause more depression.
With our new model, depression can be thought of as a multifaceted sign of chronic immune system activation. It means the immune system has been fighting in a war for a long time, maybe against a bacteria, virus or fungus, or maybe against malignant cells or dying tissue. In a similar fashion, fever is a simple sign of acute immune system activation. It means the immune system is intensely fighting in a sudden war, usually against some kind of infectious agent. Many years ago, due to lack of immunological knowledge, fever was believed to cause disease and make diseases worse. We now know fever is merely a sign of acute immune system activation and the higher the fever, the more serious the disease. With our present understanding of fever, it is absurd to think of fever causing disease. Likewise, in our new model of depression, it is absurd to think of depression causing disease. Instead, depression is merely a complex sign of chronic disease.
Next chapter: The Immune-Brain Connection
Chapter 2 References
1. Mizel SB. The Interleukins. FASEB J 3:2379-2388, 1989.